At 2 a.m. on the Saturday a week before Christmas in 2020, I woke in a cold sweat. I was dizzy, shaking, and confused, and my heart pounded like I was in the middle of a workout. Minutes passed, with my distress continuing to rise. This was no nightmare; something was wrong.
Whatever was happening, this was unknown territory for me. Other than migraines and some general anxiety, I’d never had health problems, let alone something that felt like an emergency. What even was the threshold for that? What was I supposed to do?
Blood pressure … you were supposed to take blood pressure during things like this, right? My doctor had given me an at-home cuff to monitor my BP during the short time we’d tried beta blockers for migraine prevention. Those hadn’t worked, but I still had the machine stashed in a bathroom drawer.
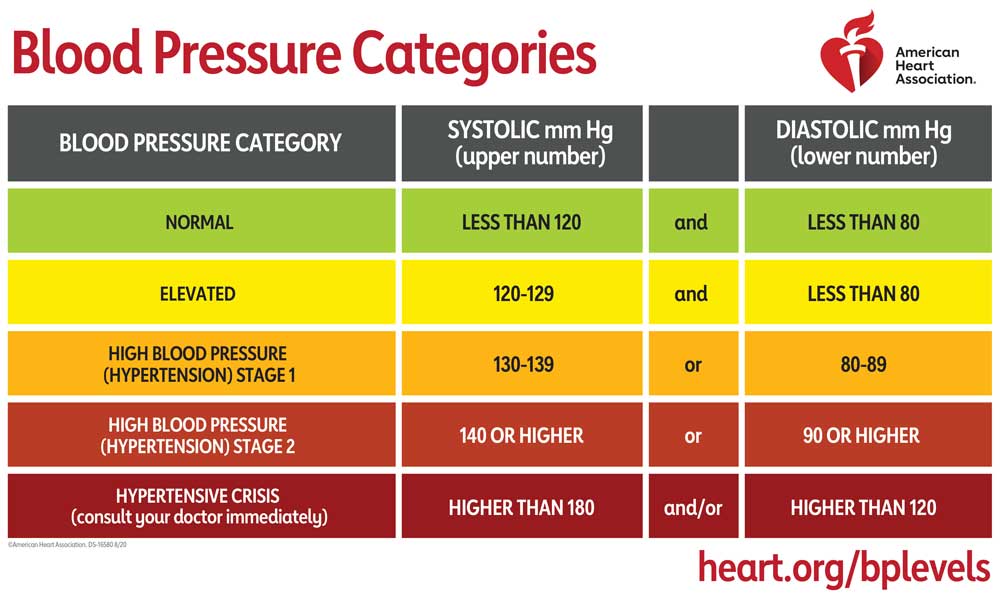
I tried to keep my breathing steady as the cuff inflated. A pause, and then the machine flashed red. Shit, that couldn’t be good. According to a cursory Google search, I was in hypertensive crisis.
I now knew the numbers justified a trip to the hospital, but I needed to consider one more thing. What on earth was this going to cost?
Night of the Living … Medical Bill
The US is undeniably the champion when it comes to outrageous healthcare bills. Us USians have the unenviable distinction of living in one of the few highly-developed countries where people routinely question whether they really need that test or doctor visit. In early 2020, nearly one third of American households said they had forgone medical care out of concern for the bill. For the millennials surveyed, the percentage was higher, coming in at 40 percent. The outlook has only gotten worse with inflation. In 2022, the overall number of Americans opting to skip care increased to 38 percent. And we’re not just talking minor sniffles; in more than a quarter of cases, care was deferred for serious ailments.
Reluctance to seek medical attention often results from deep-seated financial trauma, which in some cases persists after the insecurity has been overcome. I fall into that category. As a teenager, I was poor in the rural, midwestern sense of the word. While we always had food, shelter and working(ish) cars (an absolute necessity with the nearest grocery store 12 miles away), we lived in constant fear of any unexpected expense. A medical bill was a type of ultimate nightmare.
And forget health insurance. As a minor, I qualified for Medicaid, but I distinctly remember that they covered as little as possible. Later, in college and fully uninsured, I became adept at rationing my own care. The choice was further cemented once I experienced the medical dismissal so many women encounter; there’s not much worse than having to pay several hundred dollars for a useless doctor visit.
Joining the workforce didn’t bring much improvement. As an adjunct university instructor, I was considered part time and not eligible for benefits. When I moved on to the corporate world, I was able to get insurance, but that didn’t mean anything else changed. My employer was a cheapskate (who, it was later revealed, committed several billion dollars in tax fraud), so our health insurance came complete with a horribly high deductible, an eye-watering out-of-pocket maximum, and an “I will definitely deny that coverage” attitude towards whatever they could get away with. By the time I moved on to an employer who actually gave a shit, I’d long been accustomed to declining any but the most essential tests. And, as we’ll see later, old habits die hard.

Image by Money Knack on Unsplash
Onward to the ER! (But No Ambulance, Plzkthx)
We opted to drive the five minutes to the hospital. I’d heard the horror stories about $5000 ambulance rides,
and I wasn’t about to bring that on myself if I could help it. My husband dropped me off at the entrance; COVID protocols meant he couldn’t come in with me.
Walking alone into the emergency room during the height of the pandemic was nothing less than surreal. I had expected the waiting room to be full, like I’d been reading about on socials, but instead I found it deserted. I had been imagining having to wait, surrounded by possibly contagious people and fighting the real possibility of passing out, so the utter lack of people was somewhat a relief. However, this relief was short-lived when the triage attendant, upon taking my pulse and blood pressure, immediately called someone to walk me to a room. They practically chased me with the EKG machine and were sticking on the leads before I even crawled into the bed.

One EKG (normal), chest x-ray (also normal), some blood tests (spoiler: not normal), a saline IV, a potassium pill, and four hours of waiting later, I was sent home with the glimmer of a diagnosis. Apparently, my symptoms could be explained by a thyroid imbalance, evidenced by the fact that my thyroid stimulating hormone (TSH) was off the charts. I wasn’t going crazy, the attending physician wanted me to know. My doctor would need to do more tests, she said, but this was likely a common condition called Hashimoto’s.
(And what did all of this cost me? The bill came out to $5,000, half of which was paid by my insurance. The other $2,500, I shoveled out of my HSA and was thankful it wasn’t worse.)

Image by purple carrot nutrition, used under CC BY-SA 4.0 via Wikimedia Commons.
So, What Even is Hashimoto’s Disease?
Hashimoto’s thyroiditis is an autoimmune condition where the body produces antibodies against your own thyroid, the butterfly-shaped gland at the base of your throat. It’s an instrumental part of your endocrine system, and it controls metabolic activity as well as (you guessed it!) heart rate, blood pressure, and more. When excited (by stress or whatever the heck else causes an autoimmune flareup), antibodies go on the attack, and over time this results in a damaged, underactive thyroid. In fact, most cases of hypothyroidism are caused by Hashimoto’s, making it a common condition, especially in women.
(Incidentally, literally the week before all this happened, my doctor had asked if I wanted to run this preventative test, which would have been free under the Affordable Care Act. And guess what? I had declined for no real reason other than being in the habit of rationing my own care. I could probably have avoided that ER bill, but nooooo.)
Most people with Hashimoto’s experience it as a metabolic slowdown. Weight gain, fatigue, sometimes joint and muscle aches. These are “normal” symptoms of hypothyroidism.
I, of course, have the dubious honor of not being normal. In the early stages of Hashimoto’s, before the thyroid has undergone extensive damage, an antibody attack can result in symptoms of hyperthyroidism. The theory is that after being attacked, the injured thyroid leaks excess hormone in the blood. I’m not sure if my lab results support that, but it’s the best explanation I’ve got, so I guess I’ll just go with it.
Overall, this hyperthyroid-ish Hashimoto’s situation doesn’t seem to be common, and if you’re, say, spending the weekend furiously Googling your symptoms until you can get in to see the doctor, it can feel positively unhinged. Fortunately, my doctor had seen this before, so my bewilderment didn’t drag on too long.
During what I call a “thyroid attack,” I can look forward to:
- Sudden waves of panic while doing something completely normal (usually my first cue that we’re descending into misery).
- Tachycardia, or racing heartbeat (usually 110 to 120 resting).
- High blood pressure (often systolic over 140 to 150, with diastolic from 95 to 110).
- Dizziness.
- Chest pain (presumably because of the panic).
- So. Many. Bathroom. Breaks. (Sped up metabolism, yo!)
- Full-body tremors.
- Inability to withstand warm environments.
- Lack of appetite.
- Rapid weight loss.
- Insomnia.
- Fatigue.

The Stress Factor
It’s common knowledge (well, at least I think so) that stress can trigger autoimmune symptom flare ups. For people with autoimmune conditions, a bad week at school or the office can be rewarded with a bout of bowel distress or an increase in arthritis pain. (This can then lead to a bigger struggle at work or school the next week, a cruel, cyclic type of irony that I can guarantee is not lost on anyone battling chronic illness.)
However, the role of stress in autoimmune responses may go beyond just exacerbating symptoms of an already-present disease process. Recent research into what initiates autoimmunity in the first place has raised a damning possibility: stress itself might be to blame. To be fair, the jury is still out on whether the study’s findings – which indicated higher prevalence of autoimmune conditions in those previously diagnosed with a stress disorder – are better described as causation or correlation.
Personally, I wonder if an undiagnosed autoimmune condition might result in undue stress, rather than the other way around. In hindsight, some of my past, irrational reactions to social situations might be explained by “mini-attacks” over the years. (Again, something that might have been avoided if I’d taken the damn tests.)
Then again, I’m no stranger to work- and mental health-related stress. From school to career, I’ve faced high expectations (both self-imposed and otherwise), and my “winning” combination of procrastination and disorganization have made everything doubly difficult. If the resulting constant, low-to-medium-grade anxiety isn’t enough to trigger chronic health problems, then I don’t know what could.
As someone who deeply resents work and the mental health struggles I’ve faced since entering the workforce, I can’t deny that I’m fully, caustically bitter about the idea of my current and future health problems being caused by work. (Because of course, once you have one autoimmune condition, you’re significantly more likely to develop more in the future.)

Image by nicollazzi xiong on Pexels.
A New Prime Directive: Reduce Stress (Or Else)
That first episode in December 2020 lasted about a week, during which I slept minimally, obsessed about my blood pressure, and trembled miserably on my couch. Once I started levothyroxine (synthetic thyroid replacement hormone) things were better, but I now had the constant threat of future attacks to contend with.
And contend with them, I did. During 2021, I had several minor episodes, the worst of which started on my way home from a trip out of state. If you think air travel is stressful under normal circumstances, try doing it when you may have to urgently run to the bathroom at any given moment. (If you already experience this on a regular basis, ugh, I’m sorry!) It became clear that this was specialist territory, and my doctor referred me to an endocrinologist.
A referral wasn’t as easy as it might seem. In theory, the nationwide average wait for a new patient visit is (as of a 2022 survey) 26 days.
I suppose I don’t know about anyone else, but I’ve had to wait months on more than one occasion. This time, it was eight months. This would have been fine except for the perfect storm of stress waiting for me in January 2022.
It went like this: On New Year’s Day, one of my cats had an accident and had to be rushed to the emergency vet (a visit that was, as you can imagine, not cheap). Once home, she required hand feedings and regularly scheduled medications.

In normal circumstances, this wouldn’t have been a problem since I worked from home, but life had thrown another hurdle at me in the form of jury duty.
It was just my luck that not only did I have to report to jury duty in person (which had never happened before), I was also selected. it turned out to be the worst type of trial. That’s right, the big M. Between the cat situation and the tension of two weeks(!!) of being hustled in and out of a too-warm courtroom, the dizzy spells started up again. During breaks, I had to pace up and down the jurors’ hallway, listening to audiobooks and knowing, just knowing, that I was gonna be in for it, and soon.
Once the trial finally ended, I didn’t even make it back to work one day before I was plunged into my worst thyroid attack ever.
It was more than three weeks before I was relatively ok again. While I got lucky and there was a cancellation at the endocrinologist’s office, a snowstorm and COVID-related supply problems delayed my blood test results for more than a week, which meant that my doctor couldn’t change my levothyroxine dosage. This was not a welcome situation, as it can take weeks for dose changes to take effect.
As the storm broke and I finally emerged from the miasma, I arrived at a new understanding. Either I needed to find a way to control the stress in my life, or my body would put me out of commission. And what was my biggest source of stress? That’s right: work. My financial independence escape ladder was now a matter of physical health, not just sanity.
And that brings us to … now. This blog isn’t going to magically solve all my problems, but I think it’s well worth the effort to explore the interlinked relationships between work philosophy (both personal and societal), financial strategy, and physical and mental wellbeing. If I remember correctly, Jessica McCabe has said that she started her YouTube channel, How to ADHD, partly to create a repository of information for herself. (It’s a fantastic channel, by the way.) Learning and communicating about ADHD was a good way to cement concepts she wanted to remember, and it had the added benefit of helping other people too. I think that’s a great outlook, and so I’m going to shamelessly copy it.
This is my trash heap repository of ideas, complaints, and coping strategies. Come, ye fellow trash pandas, and forage as you see fit.







Leave a comment